Abstract
Introduction: Febrile neutropenia (FN) is defined as a temperature >100.4°F in the setting of an absolute neutrophil count (ANC) less than 1000 cells/mm3. FN carries a mortality that has been variably reported between 2% and 20%. Monotherapy with cefepime, a carbapenem, or piperacillin-tazobactam are recommended as first-line therapy. The addition of vancomycin has not been shown to reduce mortality. Overuse/misuse of the aforementioned antibiotics has been reported to contribute to the rise of drug-resistant organisms causing life-threatening infections in febrile cancer patients (FCP). Our study aims to assess antibiotic stewardship in FCP at our institution and the outcomes of infections in this patient population.
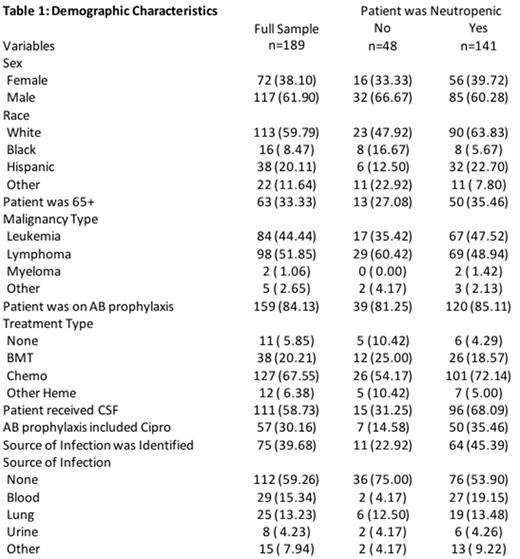
Methods: A retrospective chart review of 200 randomly selected patients with hematologic malignancies admitted with a diagnosis of fever from 1/2011 through 12/2016 was performed. Eleven patients were pediatric cases and therefore excluded. 189 adult patients were analyzed using univariate and bivariate statistics; Chi-square tests were performed to assess differences across groups.
Results: Patient demographics and characteristics of infection are shown in Table 1. The in-hospital neutropenia-related mortality (NRM) for neutropenic patients was 16% while the all-cause mortality for neutropenic patients was 39%. Neutropenic patients with leukemia had higher NRM than neutropenic lymphoma patients (65% vs. 35%; P=0.01), those who received granulocyte colony stimulating factor had lower NRM compared to those who did not (11% vs. 24%; P=0.04), and neutropenic patients without an identified source of infection had lower NRM than those with a documented infection (36% vs. 64%; P=0.00). Neutropenic patients who had a resistant organism isolated were less likely to survive their episode of FN than those who did not (56.3% vs. 95.7%%; P=0.00). There was a non-significant trend towards lower NRM amongst neutropenic patients who were on prophylaxis with ciprofloxacin prior to admission compared to those who were not (10% vs. 18%; P=0.17). There were no NRM differences amongst neutropenic patients who developed FN as a complication of stem cell transplantation versus chemotherapy (P=0.31), ≥ 65 years of age compared to <65 years of age (P=0.69), infection with gram negative compared to gram positive organism (P=0.89) or those treated with cefepime alone compared to cefepime plus vancomycin (P=0.62). Of the patients with FN, 68.8% received a cefepime-containing regimen (22.7% cefepime alone, 46.1% cefepime plus vancomycin). Of the patients that had fever without neutropenia, 45.83% received a cefepime-containing regimen (14.6% cefepime alone, 31.23% cefepime plus vancomycin). 2.1% of the population had an identified infection with methicillin-resistant staphylococcus aureus (MRSA) and 3.7% had an infection with vancomycin-resistant enterococcus (VRE).
Conclusion: Improved supportive care, including prompt administration of broad spectrum antibiotics and evidence-based sepsis guidelines, has reduced the morbidity and mortality of FN. This is evidenced by the lower in-hospital NMR compared to the all-cause mortality rate in our patient population. Nonetheless, patients infected with resistant organisms have higher NRM. The inappropriate use of cefepime in febrile, non-neutropenic patients and of vancomycin in febrile cancer patients with or without neutropenia suggests a greater need for antibiotic stewardship at our institution. As the addition of vancomycin offers no survival benefit, more judicious use of this antibiotic is warranted in FCP as its overuse is contributing to the rise of resistant organisms such as VRE. Implementation of methods such as placing holds in our institution's electronic medical record requiring calculation of ANC prior to administering antibiotics and education programs regarding the appropriate empiric antibiotic regimens in febrile cancer patients with or without neutropenia is merited.
Leslie: celgene: Speakers Bureau; KITE pharma: Speakers Bureau; seattle genetics: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal